Comprehensive Guide to Contraceptives: Methods, Function, Pros and Cons
Contraception can be a controversial topic, but regardless of your personal beliefs, it’s important to know what your options are so you can make an informed decision that’s best for you and your partner. It’s also important to be aware of the potential side effects especially of hormonal birth control, which most doctors don’t tell you.
There are four types of contraception: hormonal, barrier methods, permanent methods and family planning (which includes fertility awareness method otherwise known as the symptothermal method). I highly recommend you read my previous post about How the menstrual cycle works and 7 signs of a healthy period first to give you some background about how female hormones are supposed to work throughout your cycle.
Hormonal birth control
First things first- I want to say that NO hormonal birth control can “cure” your underlying hormonal problems such as PCOS, amenorrhea, dysmenorrhea, endometriosis, irregular periods, PMS, PMDD, etc. although most doctors and gynecologists are quick to prescribe them instead of digging deeper at the real causes of period and hormonal issues. This really pisses me off because using hormonal birth control to “fix” period and hormonal problems is a band-aid approach that can cause more harm than good long term.
The basic function of hormonal birth control is to suppress ovulation (without ovulation there’s no egg released that can be fertilized) and to create changes in cervical mucus that create a hostile environment for sperm so they can’t survive in the vaginal canal. They also prevent adequate endometrial growth so a fertilized egg can’t properly embed into the endometrial lining which prevents pregnancy. Remember: if you don’t ovulate you don’t produce progesterone which is a very important hormone for mental, bone, thyroid and cardiovascular health. Adequate progesterone function helps you sleep better, has a calming effect and can prevent against breast cancer.
Combined hormonal birth control methods include the birth control pill, the vaginal ring and the patch that contain synthetic estrogen (like ethinyl estradiol) and synthetic progesterone (progestin), whereas the hormonal IUD, Depo-Provera shot and progestin only birth control pills only contain progestin. These synthetic hormones bind to their respective cell receptors in various types of cells (fat, ovaries, etc) where they exert their physiological effects.
It’s important to note that these synthetic hormones have very different and often negative effects on the body (metabolism, inflammation, digestion, skin and mood issues to name a few) than endogenous estrogen and progesterone (i.e. hormones your body naturally produce). For example, synthetic estrogen increases your risk of breast cancer, blood clots, stroke and depression whereas progestin can cause hair loss, anxiety, androgenic properties (think testosterone excess like hair growth on your body, etc). I highly recommend reading Dr. Jolene Brighten’s book Beyond the Pill to learn more about the side effects of hormonal birth control.
It’s also very important to mention that NO hormonal birth control protects you against sexually transmitted infections so a combination of a barrier method or being in a monogamous relationship with a trusted partner is highly recommended if this is going to be your main source of birth control.
Another point I think is important to mention is that many gynecologists prescribe hormonal birth control to teenagers who complain about having irregular, “annoying” or painful periods. The problem with the widespread prescription of these drugs (yes, they’re drugs), is that women are not sexually mature in their teens and it can take 5-7 years from the onset of the first menses for the brain and ovaries to communicate with each other properly. Taking hormonal contraception disrupts this process and coming off synthetic hormones can result in hypothalamic amenorrhea because the brain and ovaries have never had the chance to communicate properly with each other to produce the proper amount of hormones throughout a woman’s monthly cycle. In fact, it’s completely normal for teenagers to have irregular or annovulatory cycles (no ovulation occurs but bleeding does occur). Puberty (and perimenopause for that matter) are hormonal rollercoasters. A teenager should see the doctor if she is experiencing prolonged bleeding for more than 8 days, no period for several months, extreme pain or frequent bleeding during the month.
While I’m at it, I feel it’s important to mention that Dr. Jolene Brighten brought to my attention in her recent Instagram post that the birth control pill was first tested on women in Puerto Rico who were used as guinea pigs without their consent to benefit reproductive technology. Moreover, the so called “feminist nurse” Margaret Sanger who made birth control available to minorities was far from a hero but rather more interested in eugenics and a fan of the Klu Klux Klan. By giving minorities access to birth control, she believed she was helping “control the population for a better society.”
Let’s also not forget that the birth control pill was developed by MEN and NOT women and there has yet to be a male birth control pill. I’m not judging anyone who takes or has taken the birth control pill. I was on it for several years. However, it’s important to shed light on female medical history (as well as the lack of studies done in women but that’s a whole other debate), so that we can start to reclaim our female health and demand for better healthcare worldwide.
Finally, on an energetic level, going on hormonal birth control often severely limits a womxn’s female creative energy and overall zest for life. If your main physical source of creativity (ovulation) is turned off, your whole energetic system is affected. I have known many women, myself included, who felt like they were in a fog, apathetic, had low libido and less creativity while taking hormonal birth control, especially the pill. So these are all things to consider before taking hormonal birth control. I don’t judge any womxn who takes hormonal birth control, but I do believe it’s important to make an informed decision before taking any medication, which unfortunately, most doctors and OBGYNs don’t take the time to do with their patients.
Metabolism of synthetic hormones
In the case of oral contraceptives, these hormones are first absorbed in the intestines, meaning that you need to have intact intestines and no inflammatory bowel disease (Crohn’s or ulcerative colitis) or history of bariatric surgery. Severe vomiting and diarrhea will also affect the absorption and therefore efficacy of the pill. After the hormones are absorbed in the intestines, they move to the liver to be metabolized by CYP 450 enzymes that breakdown via a process called conjugation ethinyl estradiol and progestin. The conjugated ethinyl estradiol (not progestin) moves into the bile where it is excreted into the colon and metabolized by a class of intestinal bacteria called the estrabolome. These bacteria produce an enzyme called beta glucaronidase that can repackage the ethinyl estradiol back into its active form where it goes back into circulation possibly leading to symptoms of excess estrogen. Otherwise the estrogen metabolites move into the feces or urine.
It’s important to note that synthetic estrogen is much more potent than the estrogens women naturally produce. It’s more taxing on the liver as this organ needs to produce more CYP 450 enzymes in order to break down the synthetic estrogen and it also causes an increase in sex hormone binding globulin (SHBG) which binds to free circulating testosterone causing a decrease in testosterone levels which often results in low libido. Womp, womp, womp. On the other hand, it can help women who have excess androgens and can improve symptoms of PCOS, hair loss and hirutism.
Ethinyl estradiol also disrupts bile transport in the gallbladder (which can cause issues with fat absorption and the absorption and assimilation of fat soluble vitamins) and may increase the risk of gallstones. Finally, this synthetic estrogen causes an increase in the production of certain liver proteins such as fibrinogen that can lead to blood clots. So anyone with a personal or family history of blood clots, stroke or Lupus should not take combined hormonal birth control especially those that have higher doses. As of now, current studies have not shown that progestin only pills pose a risk for blood clotting; however, the patch and vaginal ring appear to pose a bigger risk for blood clots than combined oral contraceptives. Therefore, bypassing direct absorption of synthetic hormones does not seem to pose any benefit in coagulation factors.
Birth control pill
Aviane, Ortho Tri Cyclin, Yaz, Nordette, Loestrin, Lo/Orval, Estrostep, Seasonique, etc
There are three main types of birth control pills:
Monophasic: these are used if you want a traditional monthly “cycle” (physiologically and hormonally it’s not a real cycle because hormonal birth control puts you in a chemical menopause in which you don’t ovulate or produce natural progesterone), and each pill releases the same amount of synthetic hormones daily.
Multiphasic: these are used for a monthly “cycle” and each pill contains a different level of synthetic hormones that intend to mimic the natural hormonal fluctuations that occur in a natural menstrual cycle.
Extended cycle: these are usually used in 13 week cycles in which you take the pills during 12 weeks and cease to take the pills the 13th week to have a medication-induced withdrawal bleed that mimics a period only because you bleed. However, a real menstrual bleed occurs from the natural fall in estrogen and progesterone that signal the body to shed the endometrial lining.
How it works
As I mentioned previously, the pill prevents pregnancy, but NOT STDs, by suppressing ovulation, preventing the production of fertile cervical mucus so that sperm cannot reach the uterus to fertilize an egg and reduced endometrial growth. A pill bleed is NOT a real period. It is a medicine-induced withdrawal bleed.
The combined hormonal contraption pill contains both ethinyl estradiol and progestin. The ethinyl estradiol suppresses FSH and therefore follicular development albeit less so in pills that have low dose hormones, reduces endometrium growth and therefore monthly bleeding and increases the action of progestins. Progestin on the other hand lowers LH levels which prevents ovulation, thickens cervical mucus so that sperm cannot reach the uterus and disrupts Fallopian tube secretion and peristalsis (wave-like movements that help push the egg down the tubes).
The progestin only pills (also called mini pills) contain about 25% the dose of progestin as combined hormonal birth control pills which means that LH and ovulation are not always inhibited. It’s main mode of action is by thickening the cervical mucus so that sperm cannot travel to the uterus. Due to its short half life (less than 24 hours), it is highly recommended that this pill is taken at the exact same time every day. Taking the pill a few hours late could reduce its efficacy. Due to the low dose of progestin only, about 40-50% of women will ovulate normally, 40% will have short irregular cycles and 10% experience amenorrhea, spotting or irregular bleeding.
Advantages:
Prevents pregnancy (91% effective)
Decreases menstrual flow
Can decrease period pain if you suffer from dismenorrea or endometriosis
Can reduce acne, migraines and ovarian cysts in some women
Fairly low maintenance. Don’t have to worry about inserting or injecting anything in you.
Lower risk of endometrial cancer
Lower risk of ovarian cancer (combined hormonal pill only)
Disadvantages
Suppresses ovulation so you don’t produce natural progesterone.
Increased risk of blood clots and therefore stroke
Causes nutrient deficiencies: CoQ10, magnesium, selenium, zinc, folate, vitamins B2, B6, B12, C and E.
Causes intestinal flora imbalances and therefore digestive issues are very common.
Depression, anxiety and low libido are very common.
Acne, migraines and ovarian cysts can be worse in some women.
Weight gain
Spotting
Vulva tissue and clitoris strinkage along with lack of fertile cervical fluid production can cause painful sex
Breast tenderness
Some women suffer from amenorrhea, PCOS and/ or acne when coming off the pill
There has also been an association with autoimmune disease risk and hormonal contraception.
Certain medications like St. John’s Wort, anticonvulsants and antimicobials might interfere with the birth control’s actions.
Increased risk of breast cancer as well as cervical cancer (when taking hormonal contraceptives for more than 5 years)
It’s very important to take progestin only pills at the exact same time every day which can be inconvenient.
Doesn’t protect against STIs.
Underlying hormonal issues are not fixed.
Vaginal ring
NuvaRing, Annovera
How it works
It’s a small flexible ring that you insert into the vagina and it releases small doses of synthetic hormones much like the combined pill that the vagina absorbs directly therefore bypassing the need to be absorbed by the intestines like the birth control pill. You keep the ring inserted for three weeks and on the fourth ring you remove it to have a medication-induced withdrawal bleed.
Advantages
Prevents pregnancy (91% effective)
Contains a lower level of hormones than most birth control pills
You don’t have to remember to take a pill daily.
Less painful than a IUD.
Can cause shorter, lighter and less painful periods.
Lower risk of endometrial cancer
Disadvantages
Carries synthetic hormones that inhibit ovulation and therefore natural progesterone production.
Irritation and/ or more vaginal secretions
Does NOT protect against STIs
Does NOT solve underlying hormonal issues
Some medications and supplements may reduce its efficacy such as Saint John’s Wort, antibiotics, anticonvulsive medication, antibióticos, the antifungal griseofulvin, etc
The patch
Xulane, Twirla, Evra
How it works
As the name suggests, it’s a small patch that you place on your inner arm, abdomen, back or buttocks and it releases both synthetic estrogen and progesterone that are absorbed directly through the skin and therefore do not need to be absorbed by the intestines . You have to change the patch every week for three weeks and the fourth week you have a medication-induced withdrawal bleed. Unlike band-aids, you can bathe, shower, swim and exercise normally without having to worry about the patch falling off.
Advantages
Prevents pregnancy (91% effective)
Contains a lower level of hormones than most birth control pills
You don’t have to remember to take a pill daily or insert anything.
Less painful than a IUD.
Can cause shorter, lighter and less painful periods.
Lower risk of endometrial cancer
Disadvantages
Carries synthetic hormones that inhibit ovulation and therefore natural progesterone production.
Skin irritation at sight where patch is
Does NOT protect against STIs
Does NOT solve underlying hormonal issues
Some medications and supplements may reduce its efficacy such as Saint John’s Wort, antibiotics, anticonvulsive medication, antibióticos, the antifungal griseofulvin, etc
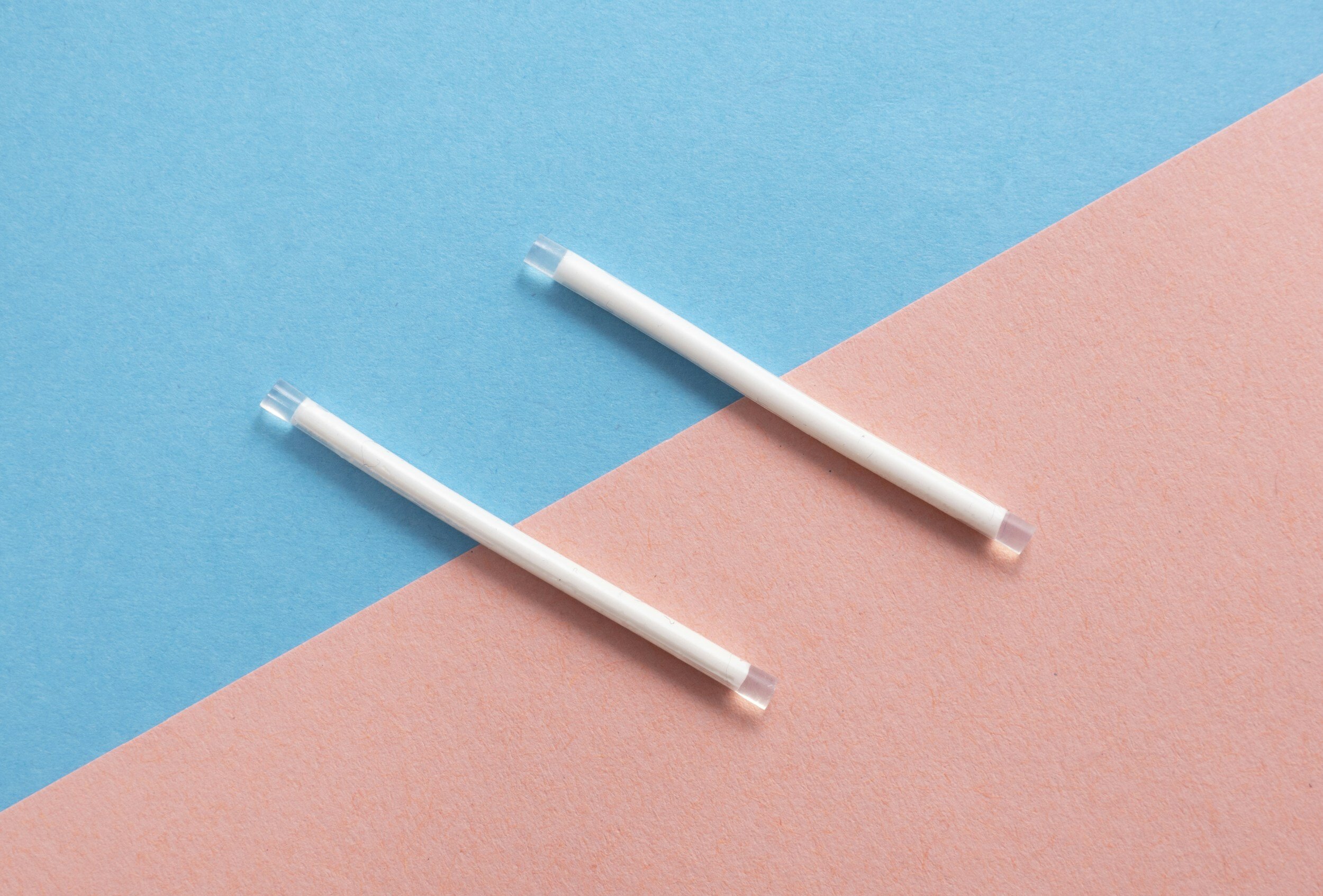
The implant
Nexplanon
How it works
It’s a small device about the size of a match that the doctor inserts in your inner arm and releases progestin only and works much like the hormonal IUD. These hormones are directly absorbed into the skin and therefore bypass the need to be metabolized by the intestines and liver. It’s main mechanism for preventing pregnancy is thickening cervical mucus so that sperm get trapped and cannot travel to the uterus to fertilize an egg. It sometimes also suppresses ovulation but not always. It also atrophies the endometrium so women experience little bleeding.
Advantages
Prevents pregnancy (99% effective)
Low maintenance: lasts up to 5 years and you don’t have to remember to take a pill daily or change your ring or patch.
No decrease in bone mineral density because it doesn’t suppress FSH or estrogen.
Contains a lower level of hormones than most birth control pills
Less painful than an IUD insertion
Can cause shorter, lighter and less painful periods.
Lower risk of endometrial cancer
Disadvantages
Need a doctor to insert it
Irritation at site of insertion
It does NOT protect against STIs.
It does NOT solve underlying hormonal issues.
Contains synthetic hormones which have their own side effects.
Hormonal IUD
Mirena, Skyla, Kyleena, Lileta
The hormonal IUD (intrauterine device) is a small T shaped piece of plastic that the gynecologist inserts into your uterus and it releases small amounts of progestin that are directly absorbed (no need to be metabolized in the liver).
How it works
It’s main mechanism for preventing pregnancy is thickening cervical mucus and sometimes also suppresses ovulation. It also atrophies the endometrium.
Advantages
Low maintenance: set it and forget it for 3 years
Prevents pregnancy (99% effective)
In most cases it causes shorter, lighter and less painful periods
It doesn’t suppress FSH or estrogen so no bone loss.
Can reduce PCOS and endometriosis symptoms
Doesn’t contain any synthetic estrogen (good for women who have issues with excess estrogen or metabolizing estrogen)
Lower risk of endometrial and ovarian cancers
Disadvantages
Contains progestin which doesn’t have the same health benefits as progesterone. Progestin can cause: hair loss, anxiety and androgenic properities.
Insertion can be painful and in some women it can worsen cramps and period pain
Doesn’t protect against STIs.
Doesn’t solve underlying hormonal issues.
Spotting is very common.
Acne, mood changes, anxiety, headaches
The IUD can perforate the uterus in rare cases.
Ectopic pregnancies can occur in rare cases.
The shot
Most commonly known as Depo-Provera
The most common hormonal shot is Depo-Provera that contains high levels of a type of progestin called Depot-medroxyprogesterone acetate that your doctor injects every 3 months. The Depo shot completely inhibits LH production and suppresses FSH and therefore ovulation, thickens cervical mucus and alters the endometrium so that in the unlikely event an egg does become fertilized, it won’t be able to successfully implant in the endometrium. There are several side effects of the Depo-Provera shot and it’s probably one of my least favorite birth control methods.
Advantages
Prevents pregnancy (99% effective)
Low maintenance: one shot every 3 months
Can shorten the length of periods
Lower risk of ovarian and endometrial cancers
Disadvantages
Contains higher levels of synthetic progestin.
Not recommended if you have a personal or family history or breast cancer.
Spotting is very common.
Bone loss is very common.
Does NOT protect against STIs.
Does NOT solve underlying hormonal issues.
Can cause decreased bone density, weight gain, headaches, dizziness, abdominal pain, fertility issues and decreased libido.
Less common side effects include: hair loss, acne, breast tenderness, insomnia and hot flashes among others.
Non hormonal birth control
While the pill and condoms are probably the most well known birth control methods, non hormonal birth control can be highly effective at preventing pregnancy without the side effects of synthetic hormones.
Copper IUD
common brand is Paragard
How it works
It works just like the hormonal IUD except it the T shaped device doesn’t contain hormones and is covered in copper which is toxic to sperm. The gynecologist has to insert the IUD and it can last up to 12 years.
Advantages
99% effective at preventing pregnancy
Low maintenance: set it and forget it and lasts for years
Does not contain synthetic hormones and allows you to ovulate naturally.
Once it’s removed, you don’t have to wait to get pregnant or have to deal with post IUD side effects as is the case with coming off the pill
Disadvantages
Does NOT protect against STIs
Insertion and having the IUD can be very painful.
Insertion and removal have to be done by a gynecologist.
Period length, pain and blood flow can be much worse and is therefore not recommended if you have endometriosis or dysmennorhea.
Can cause copper toxicity and inflammation which can elevate estrogen levels, cause mood disorders and lower zinc levels.
Can come out or perforate the uterus in rare cases.
Ectopic pregnancies can occur in rare cases.
Fertility Awareness Method
also known as Symptothermal Method
Contrary to popular belief, women who menstruate are NOT fertile during the whole menstrual cycle. In fact, healthy sperm can only survive a maximum of 5 days in the uterus. Moreover, a woman only ovulates ONE day out of her entire menstrual cycle. Women do not ovulate throughout their cycle. Leading up to ovulation, fertile cervical mucus production increases (you know those vaginal secretions you’re wondering if are a yeast infection or not) as estrogen levels rise. Fertile cervical mucus should be clear and stretchy like egg whites. The rest of your cycle your cervical mucus should be either dry, sticky like paste or creamy like body lotion.
The Fertility Awareness Method deals with tracking the changes (either on paper or via an app) of your cervical mucus, cervical position (high or low), and basal body temperature to either prevent pregnancy or try to conceive. Basal body temperature rises slightly just after ovulation when progesterone levels rise. There’s a ton of information on this beyond the scope of this blog post that you can find in the books The Fifth Vital Sign by Lisa Hendrickson or Taking Charge of Your Fertility by Toni Weschler. Lisa Hendrickson’s website and podcast Fertility Friday also offer a ton of insight into this method.
I’ve personally used this method and highly recommend it because once you get the hang of it it’s very effective and you don’t have to use hormonal birth control or invasive procedures. There is a learning curve, but once you get the hang of it after about three cycles it can be almost 99% effective at preventing pregnancy and is very low cost. The other added benefit is it forces you to know your menstrual cycle intimately and can help you detect when something is off like if you ovulated really late one month, had a longer or shorter period than normal, had a longer or shorter menstrual cycle than normal, insufficient basal body temperature rise following ovulation which could indicate low progesterone and/ or thyroid levels, etc. Overall it’s a really effective way at seeing how diet, lifestyle, stress and other factors can affect your hormones without having to due expensive testing.
Barrier Methods
Condoms are the only the only birth control methods that can protect you against both pregnancy and most STIs. Barrier methods are cheap and can be very effective IF used properly (which seems to be the tricky part for a lot of people).
Male and female condom
How it works
They block sperm from entering into the vagina via a latex (or other material for those allergic to latex) barrier. I’m sure most people know how male condoms work, but the female condom is a bit trickier to use because it requires the woman to insert one end all the way into the vaginal until it covers the cervix while the other ring covers the vulva area.
Advantages
85-79% effective at preventing pregnancies and the majority of STIs (except herpes, syphilis and genital warts)
Cheap and easy to use
Doesn’t require a prescription or medical intervention
Doesn’t contain hormones.
Disadvantages
Can interrupt the mood during sex.
You have to use them properly in order for them to be effective— only wear one condom at a time, the condom has to cover the genitals, it must be worn before foreplay.
Diaphragm
Not to be confused with the cervical cap
How it works
It’s a silicone disc that a woman inserts into her vagina that covers her cervix. Most require spermicide to be placed onto the cervical cap which adds as an extra protection against sperm reaching the uterus.
Advantages
84-94% effective against pregnancy (if you insert it before having sex) and is more effective than the cervical cap (71-86%)
Cheap and reusable
Doesn’t require a prescription or medical intervention
Doesn’t contain hormones.
Disadvantages
Can interrupt foreplay and the mood when a woman has to insert it.
It needs to be inserted correctly in order for it to be effective.
It’s more effective if you put spermicide on the diaphragm.
Does NOT protect against STIs.
It can come out during sex in rare occasions.
Increased risk of urinary tract infections for women.
Permanent Methods
These methods require surgery and are for those who are serious about not wanting to have any more kids or kids at all.
Vasectomy
An urologist closes the ducts that carries the sperm from the scrotum to the penis. It requires anestesia but is a simple and routine procedure. This method is basically irreversible so you and your partner have to be 100% sure about your family planning before deciding to undergo this surgery.
Advantages
Nearly 100% effective at preventing pregnancy
Simple procedure that usually does not cause much pain or irritation for men.
Disadvantages
Expensive
Permanent
Can cause inflammation and pain
Medical procedure that requires anesthesia
Tube Tying
This surgery is performed by a gynecologist who blocks the Fallopian tubes so that the egg cannot travel down the Fallopian tubes into the uterus. This method is permanent and is more invasive and expensive than a vasectomy.
Advantages
Nearly 100% effective at preventing pregnancy
Disadvantages
Expensive
Permanent
Can cause more inflammation and pain for women.
Medical procedure that requires anesthesia
Methods not recommended
Due to their low efficacy, these are the contraceptive methods I don’t recommend:
Pulling out method- Need I say more. This method rarely works.
Cervical cap- the diaphragm is more effective
Spermicides alone
Vaginal washes after sex
Thinking that an absent period while breastfeeding won’t get you pregnant. You ovulate before your period so it’s hard to know exactly when your first menstrual cycle will appear after giving birth. Sometimes it’s a few months and other times it’s almost a year or more.
Things to consider when considering a contraceptive
Personal or family history of blood clots, stroke, migraines, seizures, heart attacks, Lupus, digestive disorders, smoking, etc.
Convenience and ease of use
Cost
Effectiveness
Family planning- reversible or not and time it takes your hormones to regulate naturally once off hormonal birth control
If you’re looking to prevent pregnancy and/ or reduce menstrual bleeding and pain
Medication that may be contraindicated
Recommended Resources:
Fertility Awareness Method- Fertility Friday
The Fifth Vital Sign by Lisa Hendrickson
Beyond the Pill by Dr. Jolene Brighten
Taking Charge of Your Fertility by Toni Weschler